“Rethinking The Dietary Guidelines”, of course for many years many professionals supporting low carb and paleo eating approaches have been trying to have the powers that be think about what ramifications the current guidelines are actually having on obesity and health issues.
So I thought I’d pass this on to you, “Rethinking Dietary Guidelines” by Paul R. Marantz Published online 2010 December 4. doi: 10.1080/10408398.2010.526846 in Crit Rev Food Sci Nutr. 2010 December; 50(s1): 17–18. Here it is:
Many public health recommendations are not truly evidence based (Brownson et al., 2003). Although some public health decisions can and should be made in the face of inconclusive data, many should not. The need for restraint may be especially salient when considering dietary guidelines. Dietary fat recommendations are a case in point, because they may have led to significant and harmful unintended consequences.
By a congressional mandate, the US Department of Agriculture (USDA) and US Department of Health and Human Services (US DHHS) issue revised dietary guidelines every five years. The 1980 and 1985 dietary guidelines recommended the reduced intake of all fats. In 1990, a recommendation was added that < 30% of total caloric intake should come from fat. This recommendation was continued in the 1995 edition, with qualifying language removed, and stated that “the Guidelines accurately reflect current knowledge” and that “the advice is scientifically sound as well as prudent and practical” (USDA, 1995).
The 1995 edition began to recognize the disconnect between population-based trends in heart disease versus obesity and their relationship to fat intake: “More Americans are now eating less fat, saturated fat, and cholesterol-rich foods than in the recent past, and fewer people are dying from the most common form of heart disease. Still, many people continue to eat high-fat diets, and the number of overweight people has increased” (USDA, 1995). Then, in 2000, the Dietary Guideline Advisory Committee reversed its previous recommendation and suggested that the recommendation to lower fat intake had perhaps been ill advised, and might actually have some potential for harm:
Further, the possibility that over-consumption of carbohydrate may contribute to obesity cannot be ignored. The committee noted reports that an increasing prevalence of obesity in the United States has corresponded roughly with an absolute increase in carbohydrate consumption.”(USDA, 2000)
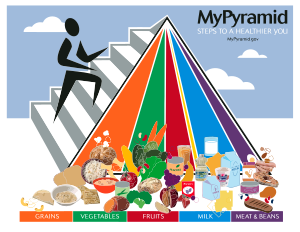
Because these dietary fat guidelines were promulgated from 1980 to 2000, relative fat consumption declined in the United States during that time. However, there was also an alarming increase in obesity (National Center for Health Statistics, 2005) and attendant diabetes (CDC, 2007). How might this disconnect have occurred? The recommendation to reduce relative fat intake produced mixed results. The major contributor to reductions in the percentage of calories from fat was not a reduction in the numerator (absolute fat intake), but an increase in the denominator (total caloric intake). For instance, absolute fat intake actually increased by 11% in women, whereas relative fat intake declined by 9%. The increase in total calories reflected increased carbohydrate consumption, despite relatively stable or declining absolute fat consumption (National Center for Health Statistics, 2005). The effective marketing of low-fat foods and the Food Pyramid, which suggested that low-fat foods could be eaten without any concern, may have influenced this trend (Taubes, 2001). Of course, the trends in marketing low-fat foods were not exclusively driven by the changes to the US Dietary Guidelines; however, our concern is that the guidelines may have provided an apparent governmental “seal of approval” for such products as fat-free cookies, which may have enhanced the appeal of these products. People might also eat larger amounts of low-fat foods; some suggest that fat intake is related to satiety, providing a biologically plausible rationale that the recommendation to choose lower-fat foods could have led to increased energy consumption (Lam et al., 2005).
Whatever the mechanism, it is clear that as dietary fat-reduction recommendations were promulgated, the relative intake of fat was reduced, consistent with the guidelines; however, total calorie (and carbohydrate) consumption increased, absolute fat intake did not substantially decrease, and an obesity epidemic began in the United States. This temporal association does not prove causation, but raises the possibility of a net harmful effect of seemingly innocuous dietary advice.
What went wrong? There are several subtleties in public health policy making that may have contributed to this scenario:
- a. Prevention through the “population strategy” (Rose, 1993) is a two-edged sword. Small benefits are magnified when applied to a large population, but so are small harms.
- b. It is important to distinguish “the public” from “patients.” Patients seek advice and recommendations, which can be individualized. Members of the public who are exposed to “guidelines” may not be looking for them, and get only “one-size-fits-all” advice.
- c. A “risk factor” is not necessarily a cause. Dietary fat may increase serum cholesterol, which is a risk factor for heart disease, but that does not mean that dietary fat reduction will necessarily have beneficial effects.
- d. A change in a specific risk factor, and a beneficial effect on a single outcome, does not establish the net health effect of an intervention. If dietary fat intake is reduced at the expense of increased total caloric intake, the net effect of these changes cannot be known without careful study.
- e. Inaction is sometimes the best option. Although emergency situations may demand action even in the setting of inconclusive evidence, dietary guidelines are not an emergency. When the evidence is inconclusive (especially considering the problems listed above), why issue guidelines?
For dietary guidelines, the strengths and limitations of evidence should be provided in easy-to-understand language. This may lead to guidelines that are laden with caveats and disclaimers, but this is preferable to resolute guidelines supported by equivocal evidence. When the evidence is murky, public health officials may best be served by exercising restraint, which is reflected by making no recommendation at all.
Guidelines may have unpredicted effects through the complexities of public perception, marketing, and behavioral changes. Because some changes may be beneficial and some may be detrimental, the net effect of these changes may be either harmful or helpful: the outcome cannot be predicted in advance. Public health, just like personal-encounter medicine, should be guided by the dictum “first, do no harm.” Sometimes, in the absence of clear and convincing evidence of net benefit, that will mean: do not issue dietary guidelines at all (Marantz et al., 2008).
Anyone want to share thoughts on this?
Related articles
- Is Fat Phobia Finally Ready To Crumble And Fall In Brazil? (livinlavidalowcarb.com)
- The Obesity Paradox: Overfed but Undernourished (civileats.com)